Mesothelioma Surgery - Surgical treatments for mesothelioma include three main types - diagnostic surgery, curative surgery, and palliative surgery. Some types of operations fall into more than one category.
For example, thoracentesis can be used as a diagnostic procedure, and as a palliative treatment to reduce symptoms. Only curative surgery has the potential to eliminate all cancers from a patient with mesothelioma.
However, for curative surgery to be effective, it is very important that mesothelioma is diagnosed as early as possible. Unfortunately, mesothelioma is usually not diagnosed until it reaches Stage III or IV, when surgery is not an option.
Surgery for mesothelioma can include pleurectomy / decortication (P / D) and extrapleural pneumonectomy (EPP). P / D removes all diseased tissue around the lungs, while EPP also lifts the lungs. Patients must be in strong health with limited cancer spread to benefit from major surgery.
For example, thoracentesis can be used as a diagnostic procedure, and as a palliative treatment to reduce symptoms. Only curative surgery has the potential to eliminate all cancers from a patient with mesothelioma.
However, for curative surgery to be effective, it is very important that mesothelioma is diagnosed as early as possible. Unfortunately, mesothelioma is usually not diagnosed until it reaches Stage III or IV, when surgery is not an option.
Surgery for mesothelioma can include pleurectomy / decortication (P / D) and extrapleural pneumonectomy (EPP). P / D removes all diseased tissue around the lungs, while EPP also lifts the lungs. Patients must be in strong health with limited cancer spread to benefit from major surgery.
Large surgery offers the greatest opportunity for long-term survival with mesothelioma. If an experienced surgeon can remove all the visible signs of cancer before spreading far away, you can live for years after surgery.
Before discussing surgery as an option, your doctor will want to make sure your body is strong enough to undergo the main procedure and recover from it. They will determine the health of your lungs and heart by performing a pulmonary function test and performing a heart test. These tests may include an electrocardiogram (ECG), stress test, echocardiogram or coronary angiogram.
If your overall health is strong enough to withstand potential complications from surgery, and your mesothelioma hasn't spread too far, your doctor will approve you as a candidate for surgery. There are risks involved in the operation, but the potential benefits are huge. Many of those who survived on Wall of Hope chose an operation that gave them longer time to spend with their children and grandchildren.
Before discussing surgery as an option, your doctor will want to make sure your body is strong enough to undergo the main procedure and recover from it. They will determine the health of your lungs and heart by performing a pulmonary function test and performing a heart test. These tests may include an electrocardiogram (ECG), stress test, echocardiogram or coronary angiogram.
If your overall health is strong enough to withstand potential complications from surgery, and your mesothelioma hasn't spread too far, your doctor will approve you as a candidate for surgery. There are risks involved in the operation, but the potential benefits are huge. Many of those who survived on Wall of Hope chose an operation that gave them longer time to spend with their children and grandchildren.
Three Objectives Are Different from Mesothelioma Surgery
Surgery for mesothelioma patients is generally divided into three categories: Diagnostics, tumor removal and palliation. Sometimes when major surgery is not an option, patients can still benefit from less invasive procedures. Choosing what type of mesothelioma surgery is up to you and the specialist who oversees your care.Statistics support surgery as the best first-line treatment option for living longer with this disease. When it comes to each individual case, sometimes the choice is clear, and sometimes the patient's condition makes it difficult to balance risks and rewards.
A mesothelioma specialist can do a thorough assessment and explain what procedure makes the most sense for your situation. They will consider several factors, including the stage of cancer and your overall health.
Diagnostic
The medical team usually cannot make a definitive cancer diagnosis without performing a small operation called a biopsy. This procedure extracts a sample of cancer cells for examination.Tumor removal
When carried out as part of multimodal therapy, major surgery to remove the tumor can prolong life expectancy and potentially send mesothelioma into remission.Palliative
Palliative surgery is a less invasive alternative to tumor removal surgery. It aims to improve the quality of life by reducing pain and other symptoms of cancer.If you qualify for surgery, you may also be able to join clinical trials of experimental treatments. Mesothelioma surgeons can offer their patients the opportunity to participate in clinical trials to investigate the best therapies to be combined with surgery. This study slowly increases the survival rate of mesothelioma.
Pleural Mesothelioma Surgery
Surgical treatment for pleural mesothelioma has improved since its inception in the 1970s. But this cancer scarcity means that most patients still need to travel to a special cancer center to see mesothelioma specialists.Diagnosing Mesothelioma Pleural and Relief Symptoms
The main diagnostic procedure for pleural mesothelioma is thoracoscopy. Two major palliative procedures, thoracentesis and pleurodesis, can also be used for diagnosis.Thoracoscopy
A thoracoscopy is also called video-assisted thoracoscopic surgery (VATS). This procedure involves inserting a special camera and a long and thin probe through a small incision in the chest. These tools allow the doctor to take a biopsy sample from the tissue around the lungs without having to open the entire chest cavity.
Thoracentesis
When fluid is formed between the two layers of the pleural layer surrounding the lungs, the doctor can drain it through a hollow needle. This procedure reduces pressure and makes it easier to breathe. Pleural fluid can then be tested for cancer cells as part of the diagnostic process.
Pleurodesis
This procedure drains a buildup of fluid, such as thoracocentesis. This then goes further by sealing the area to prevent the liquid from building again in the future. The doctor usually injects talc into the pleural cavity to seal it, although chemicals can be used in certain cases.
Removing Mesothelioma Pleural Tumors
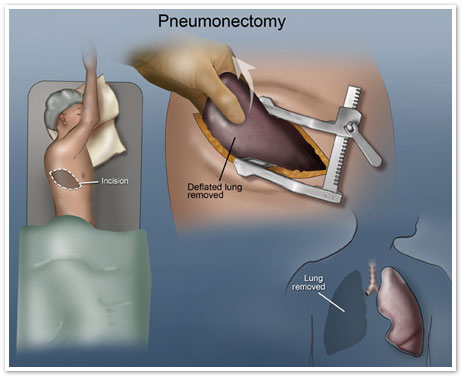
Doctors mainly use two different tumor removal surgeries for pleural mesothelioma: Extrapleural pneumonectomy (EPP) and pleurectomy / decortication (P / D). About 15 to 20 percent of people with pleural mesothelioma qualify for tumor removal surgery."Thoracotomy" is a general term for surgery that allows the doctor to access the lungs, heart, aorta, trachea or diaphragm of the patient. This involves making an incision 4-10 inches long on both sides of the chest. Extensive procedures, such as EPP and P / D, require thoracotomy. Thoracotomy is also the first step in several asbestos-related lung cancer surgeries. This surgery includes pneumonectomy, lobectomy, wedge resection and segmentectomy.
Unfortunately, up to 25 percent of mesothelioma patients undergoing surgery are found to be inoperable after a thoracotomy. Doctors are trying to predict this with the latest advances in imaging technology and other diagnostic techniques, but surgeons cannot determine whether planned tumor removal surgery is truly possible until they look into the patient.
In cases where cancer has spread too far for surgery to help, the surgeon will determine the stage of the cancer. This can guide all patient care plans. If the cancer is localized, however, the surgeon will proceed with removal of the tumor.
Pneumonectomy
This procedure involves removal of the lungs. A patient can qualify for this surgery if the cancer has not spread outside one lung. Most mesothelioma surgeons perform wider EPP surgery than only pneumonectomy.Extrapleural Pneumonectomy (EPP)
This aggressive operation removes the entire lungs, the surrounding layers, nearby lymph nodes and the pericardium and diaphragm. Theoretically, it offers the best opportunity to eliminate all cancer cells, but also permanently reduce the patient's stamina.Pleurectomy / decortication (P / D)
This procedure was developed as a less aggressive alternative to lifting the lungs. The surgeon removes the pleural layer around the lungs and all visible tumors. They erode the lungs that hurt rather than throw them away.The average hospital stay after thoracotomy is five to 10 days. This surgery irritates the nerve endings near the incision, so you may experience pain, numbness or burning under the breast and in front of your rib cage.
Drainage of clear or pink fluid from the incision is normal. You should clean your incisions in the bathroom, wash them gently with warm water and mild soap. Avoid wetting the incision in the bathtub or spa for three weeks. Avoid heavy lifting and other heavy activities for eight weeks. They can emphasize your incisions and delay recovery. You can do breathing exercises and walk every day to increase the strength, circulation and capacity of your lungs.
Robotic Surgery for Pleural Mesothelioma
Robot surgery is the latest way for thoracic surgeons to perform cancer surgery. After technology proved its effectiveness for minimally invasive procedures, doctors began using it for chest cancer surgery in 2006. In 2013, Dr. Farid Gharagozloo performed the first major robotic surgery for pleural mesothelioma patients. He used the technique to perform an extrapleural pneumonectomy.Gharagozloo is currently practicing at Florida Hospital Celebration Health. He said the da Vinci Surgical System that he used would change the future of mesothelioma treatment. Using a computer board, the surgeon can guide small instruments attached to the robot arm, allowing more precise movement. This also allows for greater magnification and better maneuverability during operation.
Robotic surgery also significantly reduces blood loss. This shortens recovery time postoperatively and decreases stress on the lungs remaining after EPP. This stress is often a big problem when operations are carried out conventionally.
Peritoneal Mesothelioma Surgery
Peritoneal mesothelioma accounts for less than a quarter of all mesothelioma cases. This is an unusual variant of cancer that is already rare. If not treated, it is also more aggressive than other types of mesothelioma. Not long ago that almost everyone diagnosed with peritoneal mesothelioma survived only six months on average.Today, however, peritoneal mesothelioma patients can benefit from one of the biggest modern advances in mesothelioma treatment: the HIPEC procedure. Nearly half of the peritoneal patients treated with a combination of special surgery and chemotherapy live beyond five years.
Diagnosing Peritoneal Mesothelioma and Relief Symptoms
A paracentesis is a minor surgical procedure that can serve diagnostic or palliative purposes. Cancer can cause fluid to accumulate in the peritoneal cavity, the space between two membranes that separates the abdominal organs from the abdominal wall. Doctors can drain fluid through a hollow needle to reduce pressure on nearby organs. Peritoneal fluid buildup is also known as ascites, and this procedure is sometimes called an abdominal tap or ascitic faucet.The doctor can check ascitic fluid to confirm the diagnosis of peritoneal mesothelioma. Ascites, also known as peritoneal effusion, often recurs with mesothelioma peritoneum. The procedure for repeated therapeutic paracentesis can be given as palliative care for patients with advanced stages of the disease.
Removing Peritoneal Mesothelioma Tumors
Nearly 40 percent of peritoneal mesothelioma patients are eligible for tumor removal surgery. The most effective treatment for this disease combines peritonectomy with the HIPEC procedure.Peritonectomy
In this procedure, the surgeon removes the diseased part of the peritoneal lining of the abdomen. Then they perform cytoreductive surgery to remove as much cancer growth as possible from the abdominal cavity. This is also called debulking surgery, and this may involve removal of the liver, pancreas, spleen, gallbladder, intestines and stomach.HIPEC treatment
Hyperthermic intraperitoneal chemotherapy (HIPEC) is given immediately after the debulking phase of peritonectomy. Mesothelioma specialists pump chemotherapy drugs directly into the abdominal cavity. They leave it there for up to two hours so that it can be absorbed by the remaining cancer cells.HIPEC has fewer side effects than oral or intravenous chemotherapy because the drug is not injected directly into the bloodstream. Targeting chemotherapy in this way allows doctors to use drugs that are far more powerful against cancer. Some chemotherapy used is absorbed into the bloodstream. But, this causes fewer side effects than intravenous chemotherapy.
Pericardial Mesothelioma Surgery
Pericardial mesothelioma patients may experience chest pain, dyspnea (shortness of breath) and coughing. These symptoms are due to a buildup of fluid in the lining of the heart. A pericardiocentesis can effectively eliminate fluid buildup to relieve these symptoms.Unfortunately, pericardial fluid rarely contains malignant cells when mesothelioma is present. This procedure is not effective for diagnosis.
Tumor removal surgery available for pericardial mesothelioma is pericardiectomy. This surgery removes as much cancer tissue from the heart layer as possible. Can relieve symptoms caused by pericarditis (pericardial inflammation) and pericardial effusion (fluid buildup in the pericardium). It is very important to treat this condition earlier, before they cause deadly complications.
A cardiac surgeon, also known as a cardiac surgeon, performs pericardiectomy. The patient must ask how many procedures the surgeon has performed to measure the level of experience of the doctor.
Certain hospitals do more operations than others. For example, a surgeon at the Cleveland Clinic followed Dr. Allan Klein, director of the Hospital Center for Diagnosis and Treatment of Pericardial Disease.
Meanwhile, Dr. Jae K. Oh, director of Cardiac Imaging and Pericardial Disease Clinic at the Mayo Clinic in Rochester, was instrumental in pericardial mesothelioma surgery performed there.
Side Effects of Mesothelioma Surgery
The most common side effects of mesothelioma surgery are pain, swelling or infection at the site of the incision. Every time a foreign object, such as a needle, knife or tube, is placed into the body, swelling and drainage usually occur. In fact, open drainage is recommended during the healing process.Mild swelling, drying and bruising on typical injured tissues. These side effects usually go away on their own within a few days or weeks.
Other side effects of surgery include:
Bloody
Most patients will experience minimal bleeding which does not pose a threat to overall health. The body will be able to regrow lost blood. During recovery, excessive stretching or damage to the incision area can cause bleeding. If bleeding becomes widespread, seek medical attention immediately.
Fatigue
Even after anesthesia is exhausted, the patient may still feel tired from the basic body pressure that occurs with an invasive procedure. This is especially true after major surgeries such as EPP or P / D. Fatigue can increase if the patient does not eat enough food or enough rest to restore the body's energy level.
Heart complications
Mesothelioma surgery performed in the chest cavity poses a risk of heart complications. The most common risks are atrial fibrillation or cardiac arrhythmias (irregular or abnormal heartbeat).
If there are excessive symptoms, you should contact your doctor. Excessive inflammation or foul-smelling drainage at the site of surgery may be a sign of infection. Other signs of infection include redness and a feeling of warmth or tingling. Postoperative infections must be controlled under doctor's care. It is very important to report the infection immediately to prevent it from becoming fatal.
Managing Pain After Surgery
Discomfort after mesothelioma surgery may be boring and tingling or more intense. For some patients, pain will occur when they stand, sit, walk or try to do daily activities. But for others, pain can occur even at rest.Your surgeon can help you develop a pain management plan to deal with the discomfort that you may experience after surgery. Before you leave the hospital, your doctor will prescribe oral pain medication.
OTC drugs can be recommended for mild pain relief. These include acetaminophen (Tylenol), ibuprofen (Advil) or naproxen (Aleve). OTC drugs should not be taken after surgery without specific instructions from your doctor.